Stem cell transplantation is frequently a ray of hope for people suffering from life-threatening illnesses like leukemia. However, in certain instances, this life-saving therapy has an unanticipated side effect called Graft vs. Host Disease (GvHD), in which the body is attacked by the cells that are supposed to heal.
Graft vs Host Disease (GvHD) Overview Table for WordPress
| Category | Details |
|---|---|
| Definition | A condition where transplanted immune cells attack the recipient’s body. |
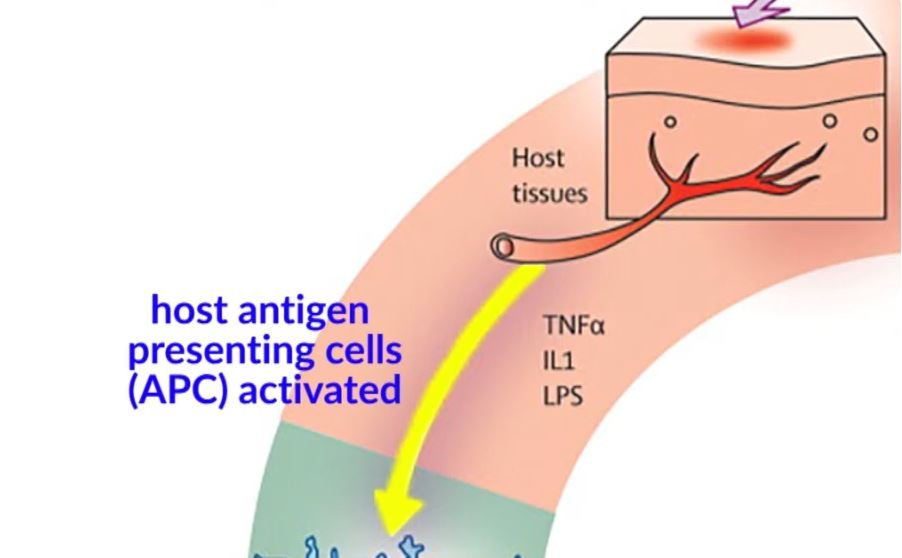
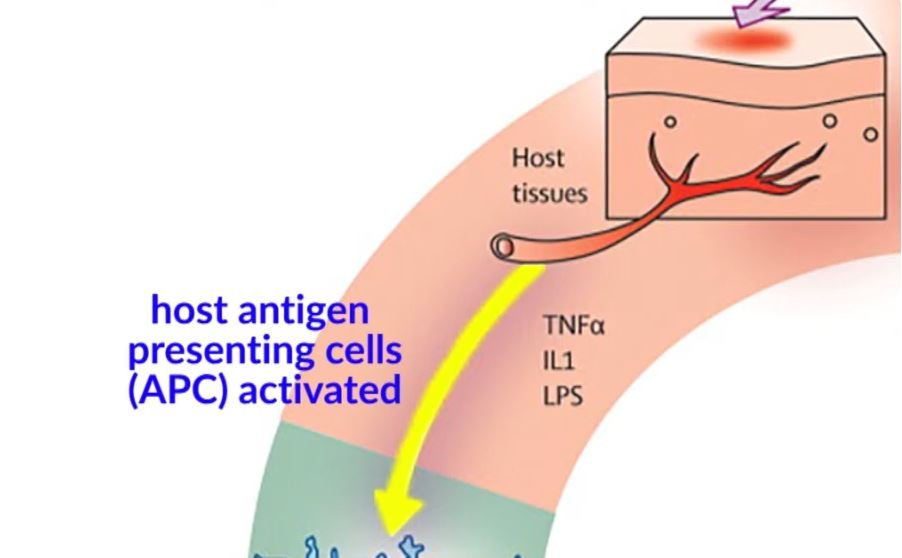
| Causes | The immune response of donor cells perceives host tissues as a foreign threat. |
| Types | Acute GvHD (develops within 100 days), Chronic GvHD (appears months or years later). |
| Symptoms | Skin rash, nausea, jaundice, diarrhea, fatigue, vision loss, organ damage. |
| Risk Factors | HLA mismatch, older donor/recipient, prior pregnancies, use of peripheral blood stem cells. |
| Treatment | Corticosteroids, immunosuppressants, targeted therapies like Ruxolitinib (Jakafi®), Belumosudil (Rezurock™). |
| Prevention | Improved donor matching, T-cell depletion, immunosuppressive protocols. |
| Prognosis | Early treatment improves outcomes; chronic GvHD can require lifelong management. |
| Latest Research | Gene therapy, CAR-T cell treatment, AI-driven precision medicine. |
How GvHD Operates: Your Blood’s Hidden Battle
Consider a skilled security force arriving in a new city. They attack it after mistaking the locals for intruders and failing to defend it. Donor immune cells perceive the recipient’s body as alien and launch a destructive attack, which is precisely what occurs in GvHD.
Comparing Acute and Chronic GvHD: An Overview of the Two Stages
There are two types of GvHD: acute and chronic. Within the first 100 days following a transplant, acute GvHD may manifest as liver dysfunction, rashes, and nausea. Chronic GvHD affects several organs, including the eyes and lungs, and manifests later in life. It can last for years.
Who Is Most in Danger? The Main Elements of GvHD
Although some factors raise the risk, not all transplant recipients develop GvHD. Peripheral blood stem cells over bone marrow transplants, an older donor, previous pregnancies in female donors, and a mismatch in donor-recipient HLA markers are all factors.
Symptoms: The Unmistakable Warning Signs
The initial symptoms of GvHD, such as a rash, dry mouth, and mild nausea, can be surprisingly mild. However, as the illness worsens, severe diarrhea, jaundice, blurred vision, and even organ failure may result. Early symptom recognition is essential for prompt intervention.
Options for Treatment: How Science is Retaliating
Maintaining the body’s defenses while suppressing the rogue immune response is a delicate balance that must be struck in order to manage GvHD. Belumosudil (RezurockTM), corticosteroids, and ruxolitinib (Jakafi®) have all demonstrated remarkably positive outcomes, aiding patients in regaining stability.
GvHD Prevention: Is It Possible?
Although GvHD cannot always be avoided, advances in medicine are greatly lessening its severity. Doctors are reducing the risk by closely matching the genetics of the donor and the recipient, using immunosuppressive medications after transplantation, and modifying the levels of T-cells in donor grafts.
The Unexpected Advantage: When GvHD Aids in the Battle Against Cancer
Not all mild cases of GvHD are harmful. In actuality, cancer patients may benefit most from it. Remaining cancer cells are destroyed by the same immune response that attacks healthy cells; this process, called the graft-versus-tumor effect, increases survival rates.
Chronic GvHD Life: Resilience Stories
Chronic GvHD becomes a lifelong struggle for certain patients. It may impact the internal organs, joints, and skin, necessitating continuous care. With focused treatments, physical therapy, and lifestyle modifications, many survivors lead happy lives in spite of these obstacles.
A Sneak Peek at the Future of GvHD Treatment
It is anticipated that scientists will transform the treatment of GvHD in the upcoming years. AI-powered diagnostic tools, gene editing, and customized immunotherapies are opening the door to safer, more accurate, and extremely effective transplantation processes.